Eye exercises can be powerful tools for improving vision when used properly under professional guidance. In vision therapy, eye exercises effectively address visual concerns like strabismus, amblyopia, eye-tracking problems, and rehabilitation after brain injuries. These targeted exercises help train the eyes and brain to work together more effectively. However, not all eye exercise claims are […]
How to Slow Myopia Progression in Children

Childhood is a critical stage for overall development, and vision plays a crucial role in helping children learn, explore, and grow. But myopia is becoming increasingly common among young children worldwide. Fortunately, there are ways to minimize risk and keep myopia from worsening. A few practical strategies to slow myopia progression in children include: Increased […]
Why Does It Hurt When I Blink My Eyes?

Blinking is something most of us do without thinking about it, however, when blinking starts to hurt, it can disrupt your entire day. Experiencing pain when blinking can make even basic tasks like reading emails, watching TV, or even enjoying time with loved ones uncomfortable. If your eyes hurt when you blink, this may be […]
What Are the Early Warning Signs of Macular Degeneration?

Macular degeneration can significantly impact your ability to perform everyday activities like reading, driving, and even recognizing faces. It’s one of the leading causes of vision loss among people over the age of 50, but it can develop slowly, meaning it’s often hard to notice until the damage is done. The early warning signs of […]
Can Kids Get Reading Glasses?

When we think about reading glasses, we often picture adults putting a pair of glasses on in order to skim through a book or a menu. But can children also need reading glasses, too? The short answer is yes! While it might not be as common, some kids benefit significantly from wearing reading glasses to […]
Can Meibomian Glands Be Restored?
If you’ve been experiencing dryness, irritation, or a burning sensation in your eyes, there’s a chance your Meibomian glands might need attention. These tiny yet crucial glands are key players in maintaining healthy, comfortable eyes and avoiding conditions like dry eye—but what happens when they stop functioning properly? Luckily, Meibomian Glands can be restored, especially […]
Can an Optometrist Diagnose Macular Degeneration?

Macular degeneration is a leading cause of vision loss among older adults, affecting 2.5 million Canadians. This condition affects the macula, the central part of the retina. The macula is responsible for sharp, straight-ahead vision and is vital for tasks such as reading and driving. Using targeted tools and tests, an optometrist can indeed diagnose […]
What Are Disadvantages of Cataract Surgery?

Cataract surgery restores cloudy vision caused by cataracts—a condition that affects the lens of the eye. Like any medical procedure, surgery for cataracts comes with its own set of risks and potential downsides. If you’re considering cataract surgery or are simply curious about the procedure, it’s important to be aware of both its benefits and […]
Are Glaucoma & Macular Degeneration the Same?

Eye health is a critical aspect of our overall well-being that often gets overlooked. Two common eye conditions that are frequent causes of confusion are glaucoma and macular degeneration. While both conditions affect vision and are more prevalent with age, glaucoma and macular degeneration are distinct eye conditions with different symptoms, causes, and treatment options. […]
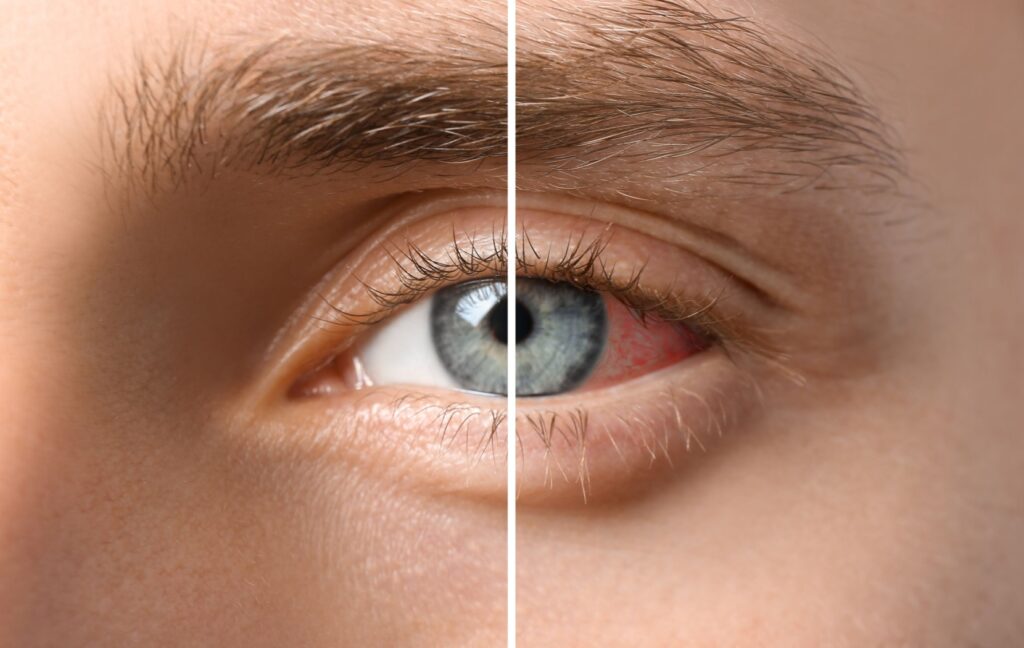
Can Chronic Dry Eye Cause Floaters?

When it comes to eye health, understanding the nuances can be a bit challenging. Two common issues often discussed are dry eyes and floaters. But can these two be interconnected? Let’s explore. What are Dry Eyes? Dry eyes occur when your eyes don’t produce enough tears or the tears evaporate too quickly. This can lead […]